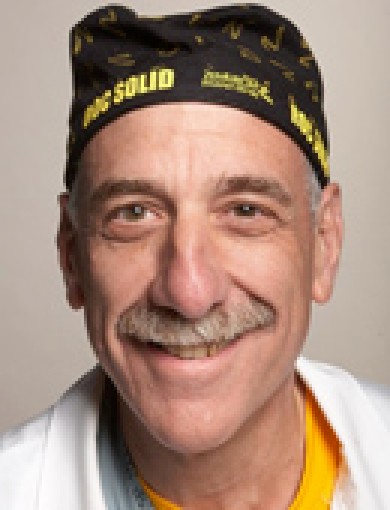
The following is a first-person account of Doctor Gaetano Bello, an attending physician in the obstetrics and gynecology department for Mount Sinai at Elmhurst Hospital. Bello is responsible for teaching the residents who rotate between Mount Sinai Hospital and Elmhurst Hospital. He is also in charge of the labor floor at Elmhurst.
The doctor’s story began the week of March 23 when he was on 24-hour call at Elmhurst Hospital and when his son, a Queens ADA, had coronavirus-like symptoms.
March 23
“A week ago Sunday, I was back in the emergency room multiple times, including with my son, who had been sick for four or five days and made me aware of it Saturday night. He had contacted the Department of Health with his symptoms: a pretty bad cough, high fever of 102, spiking higher to 104,” Bello said.
According to Bello, the DOH asked his son if he had shortness of breath. When he said no, they provided him with a number for the Department of Motor Vehicles to set him up with an evaluation and test, but they never called him back.
“When he called me Saturday night, I told him, ‘I’m gonna be at Elmhurst 24 hours on Sunday. Meet me there. I’ll take you to the emergency room and get you registered,'” Bello told his son.
When his son arrived at the hospital, Bello told the administrator in charge of the COVID area that his son was there and described his symptoms.
“He has a terrible cough for three or four days, high fever, sore throat. Not short of breath,” the doctor said. “I said, ‘I really need you to swab him because I’m sure he has COVID.'”
The administrator along with the rest of the staff said that they could only administer tests to those who were to be admitted to the hospital.
“That doesn’t make any intuitive sense because if they’re that sick, you can assume they’re positive and you’re going to treat them appropriately anyway. So why would you test those people when you should test people who you’re going to dismiss and have go home to self-quarantine, because then you can work on evaluating the people that those people have had contact with,” said Bello.
After about four and a half hours, with about two hours waiting in a room with COVID-positive patients, they cleared Bello’s son to go home “with no treatment and with a 102 fever.” His son then went home to rest with instructions and a prescription for medication, which the doctor himself prescribed.
Meanwhile
In the meantime, Bello continued doing his job at the hospital, taking care of the labor for high-risk patients and going to the police department, where he serves as an NYPD police surgeon at the pregnancy medical district.
“I spent three or four hours at the police and then I went home Monday afternoon. I did not feel ill at all. I touched base with my son, he was home, still having a bad cough but [doing] ok. Still no shortness of breath.”
His evening went by and he still felt asymptomatic. On Tuesday, March 24, he went to work at Elmhurst and at the NYPD and also scheduled office hours for a few of his patients on Wednesday.
At around midnight, he began feeling “feverish” with a hot sensation on his face but a cold body. Around 1 a.m., his symptoms progressed and he recorded a temperature of 97 degrees which he described as “startlingly low.”
Around 2 a.m., all the muscles in his body began feeling “really achy.” So he decided to call the NYPD to inform them of his symptoms and let them know he would not be coming in. He did the same with his patients and also his department at Elmhurst Hospital.
He spent the next two hours cleaning every surface and high-touch point in his home with Sani-Cloth wipes, worried for his wife, children, in-laws and grandchildren who were quarantined with him at his house.
“I told my wife, ‘Stay away from me. I’m pretty sure I’m coming down with this,'” said Bello, who has been self-isolating and resting at home since recovering from his COVID-19 symptoms.
He did not initially get tested for the virus but “knew he had it” due to the “classic symptoms.” On March 29, he received a COVID test and is currently awaiting those results. The doctor said that he is following official health guidelines to self-quarantine for 14 days.
So far, he reported that no one in his home is ill or has contracted COVID-like symptoms. While at home he has been reporting his temperatures to the occupational health department at the hospital.
Most of his recorded temperatures have been relatively low, in the high 97 and low 98-degree range. His fever reached 101 degrees on Friday, which is the highest he’s had since becoming ill.
Flattening the Curve
“Things seemed to be kind of coming apart the third weekend of March at Elmhurst where we just couldn’t have enough people there seeing patients, evaluating them and trying to triage them to different areas or back home,” said Bello.
Since that week, when 13 patients died of COVID-13 within 24 hours, the city sent additional personnel and supplies to the hospital including 169 clinicians, ventilators and masks.
“But it’s still not too late now because if we ferret out other people at risk and we get them tested and then we do medical epidemiology follow-through, we can do a better job of ‘flattening the curve’ and letting this thing not really peak the way they believe it will in two or three weeks,” said Bello.
He believes that Elmhurst, along with other hospitals, should be testing on more of a “common-sense basis,” meaning administering tests to those showing obvious symptoms of the virus including a high fever, a sore throat, signs of respiratory infection and a dry, hacking cough.
“You could be identifying a lot of people who would otherwise be missed and be contagious to other people who may not handle the disease as well should they get it,” he said.
He added that in the case of people like his son, hospitals should not be sending patients home who are exhibiting those kinds of COVID-like symptoms.
“A good number of those people, three to four days later may end up in another hospital on a respirator. That’s not what you would want to happen.”