When the blue WellCare RVs roll through the streets of several Queens communities, they stop traffic. Not because of their immense size or bright blue hue, but because it is clear that the vehicles come with a purpose—to educate residents on their options for affordable, comprehensive healthcare and provide preventative medical assistance to low-income families and the elderly.
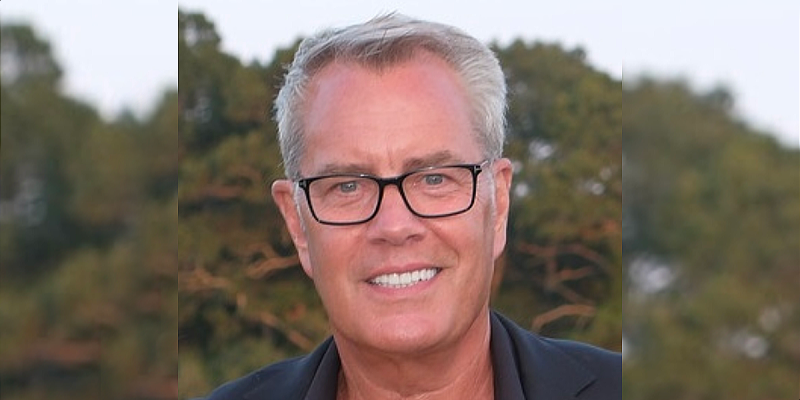
WellCare Health Plans, Inc., in business for over 20 years, is a leading provider of cost-effective managed care services for government-sponsored healthcare programs such as Medicare and Medicaid. Serving more than 2.3 million members nationwide, WellCare takes pride in investing in each individual neighborhood and community through personal outreach about prescription drug plans, Medicare Advantage plans and Medicaid health plans for families, children and the elderly and disabled. “We understand our membership and the communities we serve,” says Dan Parietti, president of WellCare New York since 2002, speaking to the personalized attention that is given to New Yorkers seeking care.
According to Parietti, what makes WellCare stand out from larger healthcare providers is the team’s approach to helping people understand their options. WellCare focuses on educating people about insurance options and investing in coverage at lower rates, while emphasizing preventative care. “We serve specific communities,” Parietti says. “We focus on the needs of specific communities and the ethnic groups and neighborhoods within those communities.” Parietti emphasizes that WellCare maintains strong relationships with the doctors and senior centers within each Queens neighborhood that it serves, further connecting them to the residents they reach out to. Under Parietti’s leadership, WellCare’s membership has quadrupled since 2002, a success he attributes to a strong management team. Parietti’s leadership has also seen the launch of the New York Medicare product in ten other counties.
Medicare Advantage allows members to access the traditional benefits of Medicare along with added benefits, such as lower co-payments and hearing, vision and dental care. Other coordinated care benefits include more flexibility with prescription drug coverage and the option of choosing a WellCare health plan with a built-in drug benefit. Additionally, Private Fee-For-Service plans are offered, in which members may see any Medicare-eligible physician that agrees to accept WellCare’s terms and conditions of payment. Private Fee-For-Service plans may include improved dental, vision and hearing coverage, along with Part D prescription drug coverage.
Recognizing the financial stress that comes with high-cost prescription drugs, WellCare offers stand-alone Part D prescription drug plans with low premiums and low co-payments.
Under Medicaid, WellCare provides health plans to participants in the federal Supplemental Security Income (SSI) program and the Temporary Assistance to Needy Families (TANF) program. While SSI is available to the elderly, blind and disabled and TANF for low-income families with children, WellCare recognizes the necessity of providing these groups with the means for quality care. By opening the doors to extensive and thorough care for members, WellCare aims to improve and maintain the health of members, therefore reducing long-term government cost. WellCare participates in the State Children’s Health Insurance Plans, which provides vaccinations, healthy check-ups and prescription drug coverage for infants, children and teens.
Parietti said he is also excited about entering the Managed Long Term Care market. “Managed Long Term Care is an exciting venture for WellCare,” he said. “Our programs have been designed for people who need health and supportive long term care services, like home care or personal care services. These services help members stay in their homes and communities as long as possible.” The two managed long term care products, known as Advocate and Advocate Complete, were first offered in late 2007. They are for Medicaid eligible or Medicaid/Medicare eligible persons, and partner each member with a Care Manager who assists the member with both health and long term care needs.
Preventative care is a top priority of many WellCare plans. Since dealing with potential medical conditions before they become a problem helps to reduce the cost of medical care down the line and improve patient outcome, WellCare recognizes that regular doctor visits are essential. Regular doctor visits also aid in the management of chronic conditions and therefore are encouraged as a way of taking advantage of WellCare’s preventative care, according to Parietti. With each managed care plan, patients are set up with a primary care physician who will coordinate and oversee their treatment and develop a specific care plan.
WellCare’s standard of preventative applies to children as well, and early start initiatives are plentiful. The Early and Periodic Screening, Diagnosis and Treatment (EPSDT) program is designed for young children with the goal that children enrolled in WellCare plans are healthy and without any undiagnosed medical conditions. The WellCare team identifies which enrolled children have not had preventive doctor visits and follows up by sending a letter to the home, asking the parent or guardian to take the child to his or her physician for a check-up. Phone calls to the parent or guardian as well as the physician are standard to ensure that the need is met.
Though only government-sponsored care programs are offered, adding to WellCare’s tailored services for each community is the decentralized model of operation. Recognizing that the populations of each neighborhood, town and city have its own needs, WellCare customizes programs to meet the needs of local members.
According to Frank Pistone, regional vice president of Medicare sales, Jackson Heights, Corona, Flushing and Astoria are primary WellCare locations in Queens, but the company is looking to expand further into South Queens, including Jamaica. In these areas, Pistone says, WellCare conducts health fairs, street fairs and seminars to help promote its plans, and the fleet of WellCare RVs and several retail hubs distribute information about prescription drugs to Queens’ residents. “What we’re finding is that there are a lot of seniors who don’t know about these plans,” Pistone says. “They are excited about it because they will be saving money and getting additional coverage.”
Additional WellCare New York offerings include home delivery of meals to seniors who are unable to grocery shop and pre-paid pharmacy cards with plans designed for eligible markets. Such pre-paid pharmacy cards allow recipients to buy the most basic drug-store necessities, like aspirin or band-aids, which they would otherwise not be able to afford. Parietti says, “We’re always looking for ways to improve the quality of lives of our clients.”
Making quality improvements to the services provided is a top concern for WellCare New York, and there are several ways that the management team goes about assessing what improvements need to be made. Member satisfaction surveys and a process of grievances and appeals for both members and providers are the most basic ways of obtaining feedback from the people who comprise the essence of WellCare. Customer service telephone lines are staffed seven days per week for 18 hours a day. Site audits of providers and providers’ patient medical records ensure that all WellCare physicians and specialists are providing quality care. Just as educational services are provided for WellCare members, providers complete education programs and credentialing as well.
As Pistone and Parietti say, effective partnerships with WellCare providers has been key in the company’s success and reputation among enrolled members. High-quality and cost-efficient care is a prerequisite for developing and expanding WellCare’s network of providers. Physician’s proximity to members, the languages spoken within their practice and medical experience are also factors. WellCare maintains relationships with providers by operating a centralized management process in which claims are processed quickly and accurately. An online provider site allows providers to check member eligibility, process claims electronically, check authorization verification and track claims status.
It is standard practice at WellCare to maintain a fluid medical management system that keeps communication open between the WellCare medical team and providers to ensure that each member receives the best possible care that can be provided. Working together with providers, the medical management staff monitors members with high-risk conditions like diabetes and asthma to coordinate care and answer their questions.
Pistone urges members to consider the case of an asthmatic patient who has not refilled a prescription for an inhaler. The WellCare medical management team reviews pharmacy records and will call the doctor to notify him or her that the patient may need additional help. “This approach is designed to improve medication compliance and reduces the number of emergency room visits,” he says. Other active approaches to monitoring members’ wellness include reminders sent out about cancer screenings like mammograms and pap smears and the identification of high-risk pregnancies to provide in-home nurse care during critical weeks.
For more information on health plans and care, visit www.wellcare.com, the official site of WellCare New York and WellCare Health Plans, Inc. The comprehensive site allows users to access information on doctors, hospitals and pharmacies, as well as detailed descriptions of the plans that will help determine which option is best for you and your family.