Remember folks cheering and banging on pots and pans across New York City’s neighborhoods in support of healthcare heroes? These three Queens-based healthcare facilities were voted Bethpage Best of the Boro, and have touched New Yorkers’ lives in a big way during the coronavirus pandemic, and beyond: St. John’s Episcopal Hospital, winner of Best Hospital; CityMD Urgent Care, which took home the award for Best Urgent Care Center; and The Woman’s Health Pavilion, winner of Best OB/GYN.
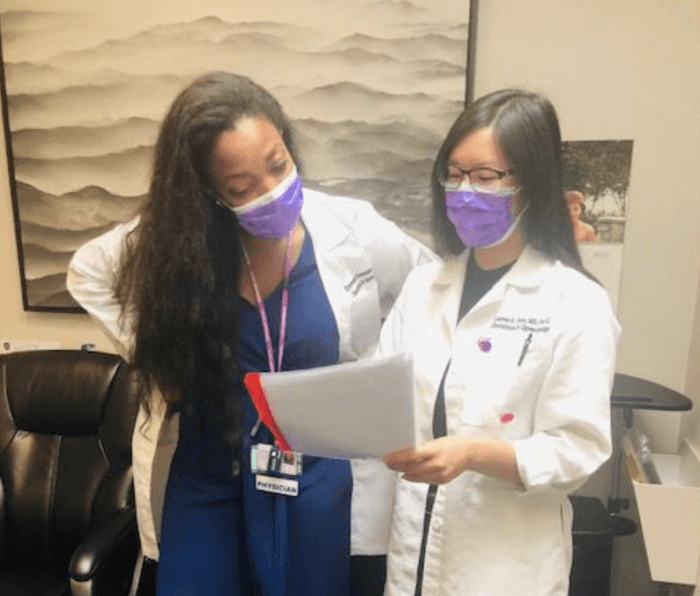
Working tirelessly at those stellar facilities are doctors, nurses, and other healthcare employees who deserve recognition for their courage and dedication, as they continue to help patients heal while ensuring everyone’s safety.
Spotlighted here are several physicians from the winning facilities, who fought on the front lines during the height of the pandemic. Juggling work and home life, they’ve been dealing with stressful, high-risk situations on the job, while keeping their families safe.
They were eager to share their personal experiences.
BEST OB/GYN
Kindhearted doctors bring families together with ‘virtual’ births at the Woman’s Health Pavilion
Well-known for their excellence in maternity care, LIJ/The Woman’s Health Pavilion (Forest Hills, Howard Beach, Long Island) is proud of their team of highly qualified and caring physicians, nurse practitioners and physician assistants, who continue to work tirelessly to keep moms and babies safe during the pandemic.
Osasumwen Asemota, MD

“One of the most memorable experiences I remember during the height of the pandemic was trying to recreate the human connection of the delivery process virtually. Mothers were not allowed to have anyone at bedside that may have symptoms or have had high risk exposure of COVID-19,” recalled Dr. Asemota, who works at the Forest Hills location and occasionally, in Westbury.
Unfortunately, the dad-to-be had COVID-19 and couldn’t come to the hospital to witness the birth of his first child. The patient was understandably very distraught, as this would be her first time delivering a baby and not being able to share this experience with a loved one, according to the doctor.
“She really desired him to be ‘there’ with her, even if it is through the phone,” Dr. Asemota said. “The husband was able to FaceTime his wife when she was pushing (from the waist up of course!) and help her with her counts and breathing. Again, although uncanny, the family really appreciated their ‘virtual’ delivery. That experience really highlighted the importance of human connection and presence, especially during these difficult times.”
After long days helping patients, family life posed its own challenges.
“I was fearful of being a carrier, especially working in the hospital. My parents are just at the cusp of being considered the vulnerable age group, so I wanted to reduce their chance of getting the virus,” she shared. So the tired doc would change out of her clothes in front of her Jamaica, Queens, home, disinfect doorknobs and countertops daily, and eat dinner separately for a while.
“I’m always in awe of the resilience and fortitude of my coworkers who also worked during the pandemic, with little information and some degree of uncertainty, but strived with this desire of helping as many people as possible,” Dr. Asemota continued. “I drew strength from their courage, as well as the hope for a better tomorrow.”
Eronmwon E. Oronsaye, M.D., M.S.
Recalling her challenging experiences early on during the outbreak, Dr. Oronsaye likened it to “entering a warzone.” She said a typical day was, arriving at the hospital and donning PPE “to ready yourself for what felt like a war.”
While sitting at the physician workstation, she would hear overhead announcements every 30 to 60 minutes, often requesting emergency personnel for patients succumbing to their COVID-19 illness.
“The baseline high-stress environment of keeping mothers and babies safe [back then], was now compounded by the ever-growing fear of contracting a potentially fatal virus,” she said. Having CoV-2 positive patients became a normal occurrence.
The mother of two found that balancing work with family life was tough as well, but said her kids were surprisingly well-adjusted to the pandemic.
“My 5-year-old was finishing up the latter half of pre-K when the pandemic struck. This created the challenge of effectively administering his remote learning activities all while working full-time. Luckily, I was able to succeed at this, despite the challenges,” she shared.
As she heals emotionally, Dr. Oronsaye also shared her new mantra for dealing with stress: “Just keep pushing,” she offered. “I was forced out of my comfort zone and nothing was guaranteed: not job security, not one’s health and wellness, not some semblance of the world that once existed. However, pushing through times of turmoil just paves a path to better days ahead. I have been making a point to cherish every day and to love my loved ones as if our time may end abruptly.”
She added, “I believe that virtually any healthcare worker experiencing this pandemic can agree that the support we have provided one another has been unmatched. We worked together as united fronts, placing our lives at risk on a daily basis, to provide care to those that needed it.”
Andre Saad, MD
Dr. Saad is president and CEO, and his priority is keeping his staff and patients safe. He stated it was a challenge of a lifetime.
“Personally, I spend most of my time performing elective gynecologic surgery. Since elective surgery was canceled in NY for three months, I was not on the front lines of the pandemic like some of my colleagues. Still, I’ve never worked harder in my life,” Dr. Saad shared.
There was no road map for navigating the challenges they faced as a practice: “How do we remain available for patients who need us, but still maintain a safe office environment? How do we get our hands on supplies that suddenly became scarce? How do we pay the practice’s bills when half of our income disappears?”
He added, “I’m so proud of the clinical team, who literally risked their lives during this crisis. I’m also proud of the support staff, whose work behind the scenes kept us all safe and kept our offices open.”
The Woman’s Health Pavilion is located at 109-33 71st Rd., #2G, Forest Hills, Queens, and can be reached at 718-263-1963 or you can visit www.ilovemygyn.com for more information.
BEST URGENT CARE CENTER
CityMD’s Dr. Matthew Mavroson keeps fighting the good fight against COVID-19
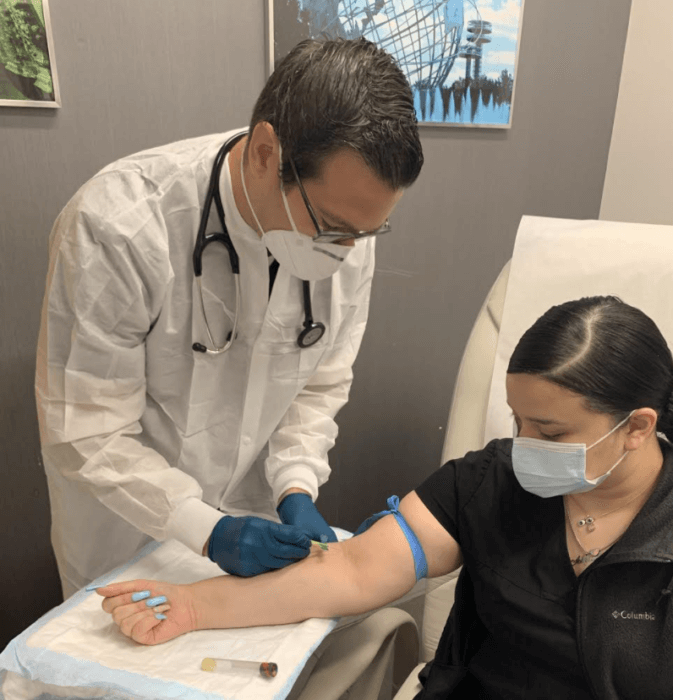
Well-known for providing top notch care to all New Yorkers, CityMD Urgent Care has evolved with the changing demands of this public health crisis. They will continue to do so until they can successfully beat the virus, according to Dr. Mavroson. In addition to COVID-19 testing, their facilities handle routine urgent care needs while helping patients during flu season.
A Board-certified physician in internal medicine, Dr. Mavroson is committed to serving the diverse communities of Jamaica and Astoria. Early into the pandemic, he helped a family at the Astoria facility. A young adult patient served as the interpreter for his family.
“He lived with his sister, parents and grandparents. They all lived together as a multigenerational family in Queens, a common occurrence in the five boroughs,” the doctor recalled. “The grandparents were observed to be critically ill, gasping for air; the parents were having shortness of breath, and the son had a low-grade fever. It appeared that he likely brought this illness home, which quickly and progressively spread throughout his household. The grandparents needed to be sent to the ER.”
The compassionate doc spoke with the son nearly every day to check in on them. Sadly, both grandparents passed away after a short time on ventilators, as did the father.
“My colleagues and I saw the devastation COVID-19 can cause to families, firsthand. I’ll never forget it,” said Dr. Mavroson, who is a devoted dad.
A typical day during the height of the pandemic started at 7 a.m., when the patients began to show up in droves, and ended near midnight for the dedicated physician, who described it as “a relentless onslaught of desperate and scared patients” from open to close.
“Every third patient or so was hypoxic (low oxygen), short of breath, and had a typical COVID-19 pneumonia pattern. I will never forget the time we were told by 911 operators that there were no available EMS for transport, leaving us no choice but to continue monitoring the patient until they arrived 90 minutes later,” he shared.
Medicine was stretched thin and resources were limited. But CityMD Urgent Care rose to the challenge.
Multiple locations of CityMD Urgent Care can be found at www.citymd.com.
BEST HOSPITAL
St. John’s winning team help patients and communities during pandemic
Celebrating over 110 years of community care, St. John’s Episcopal Hospital provides people of all faiths with high-quality medical treatments and services regardless of ability to pay. Their dedicated team of healthcare workers and staff have all been working together to save lives during the pandemic.
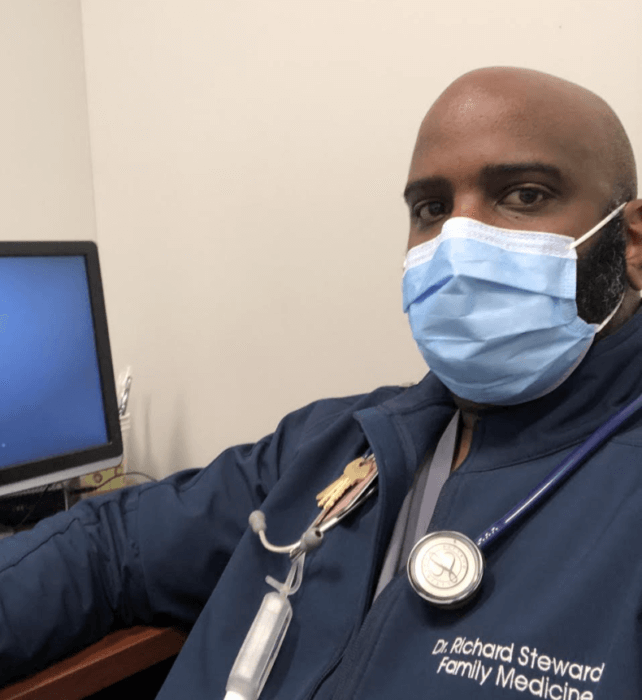
Richard Steward, DO, Family Medicine
Dr. Steward started working at St. John’s in 2015 and says he’s proud to be a part of that team. He remembers the challenges he and his colleagues faced when Queens was the epicenter of the coronavirus pandemic. Many patients were being admitted as the weeks went by, and new rooms had to be created to accommodate the influx.
As the only doctor in his family, Dr. Steward said his family members are quick to call him for advice. He shared a personal experience: “I had two cousins who came down with COVID-19 and developed shortness of breath and decreased appetite. Their families had called me on a daily basis, asking for advice on how they should manage their current condition. Their health worsened, but I was able to guide them on how to best manage their condition to help ensure that they did not deteriorate. Ultimately, they had to be admitted to a hospital. I was able to be a part of their care plan and communicate with my family’s medical staff while they were hospitalized. I was able to see them come through to the other side of this terrible virus.”
After a long, grueling day, Dr. Steward said when he got home, he could finally interact with his family around 8:30 p.m. There were times when he was at the hospital every day of the week. “I’ll never forget that during one stretch, I had worked 27 out of 30 days in the month,” he recalled.
In the midst of everything, nobody could escape conversations and news about the virus.
“My children, who are ages 7 and 13, were very aware of what was going on. Their days were difficult because they had never gone so long without having interaction with their friends. I didn’t talk much about my day with them because I wanted the time that I spent away from work to be family time,” Dr. Steward shared.
To deal with all the challenges he faced, the doctor would often remember something he once read in college.
“I learned a poem called ‘See it Through.’ In life, things will not always go the way you want, but sitting and moping around about circumstances is not going to change the situation,” he said. “The poem states, ‘Black may be the clouds about you and your future may seem grim, but don’t let your nerve desert you … if the worst is bound to happen, spite of all that you can do, running from it will not save you. See it through.”
Plus, working out at home helped him decompress and stay fit.
Dr. Steward also talked about the current ‘vibe’ in the hospital: “Healthcare workers have been wearing PPE since March as regular protocol. However, most could never have imagined that we would still be wearing it,” he said. “Wearing everything that we do for hours upon hours for months can be annoying and uncomfortable, but I still do it to protect my patients, my family and myself.”
Thomas Meyer, director of engineering

As an important part of St. John’s winning team, Meyer describes what it was like during the height of the pandemic and what he learned from that experience.
“Once your back is pushed to the wall, you can really see how much you can get accomplished. Collective ‘brain’ and manpower made so many things happen,” he said. “We can definitely come together and step up for the well-being of our patients and community members.”
Indeed, there was a lot to get done during those chaotic weeks. There were long days, constant tasks … things people may not even think of when it comes to maintaining a building.
“Engineering’s main job was to expand and create areas of space in order to keep patients and the hospital’s team members safe,” Meyer noted. “We were able to create negative pressure rooms that help prevent the spread of airborne diseases, such as COVID-19 and the flu, for the rooms of patients who were COVID-19 positive. Creating new rooms or expanding in necessary areas was a hurdle to overcome, but we knew this was needed to help reduce the infection rate. The experience was challenging, but we knew it was for the greater good.”
Everyone pitched in and there was a real sense of community and fellowship.
These days, Meyer said he has been educating himself on how to prepare for the future, including a possible surge, and feels there is a heightened sense of awareness at St. John’s.
“On a daily basis, there were a lot of things that were presented [back then] which was out of our regular scope of work, but we worked aggressively to expand and accommodate efficiently and effectively,” he recalled. “I was able to really understand the important values of team, community and individual care.”
St. John’s Episcopal Hospital is located at 327 Beach 19th St., Far Rockaway, Queens. The hospital can be reached at 718-869-7000, or you can visit www.ehs.org for more information.




































